Policies That Limit Emergency Department Visits and Reimbursements Undermine the Emergency Care System
jamanetwork.com
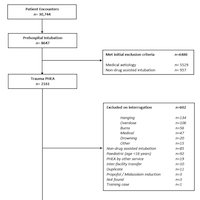
Emergency department (ED) visit rates in the United States have been rising over the past 2 decades, outpacing population growth.1 These visits are portrayed in the lay press as unnecessary visits that must be reduced or avoided. Yet a growing body of evidence indicates that most ED visits are medically necessary and that EDs serve as a critical source of care for high-risk patients, including those with comorbid mental health diagnoses, substance use disorders, and poor social determinants of health. Insurance companies and other payers have a years-long history of attempting to dissuade individuals from using the ED by refusing to pay for their visits—after the visit occurs—if it is categorized as nonemergent. In 2012, the Washington State Health Care Authority attempted to pass legislation stating they would only pay for ED visits for Medicaid patients that they deemed to be medically necessary.