ECG Pointers: Cocaine and ST Elevation
emdocs.net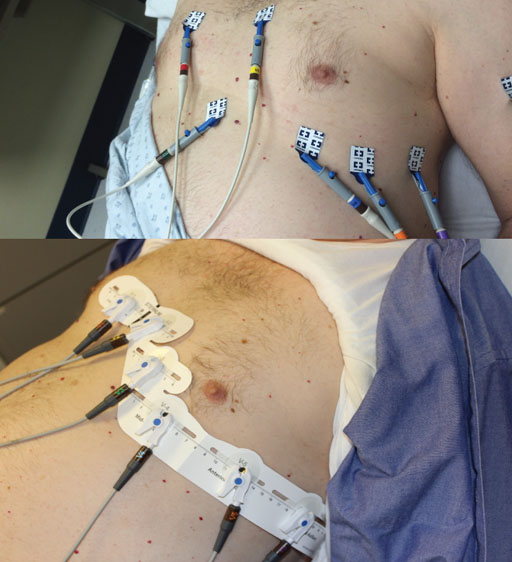
This ECG comes from a 21-year-old male with a history of cocaine abuse. When I say ‘history’, I mean that he just snorted some cocaine and now he has chest pain. He looks uncomfortable and sweaty, and keeps asking you not to tell his mom that he does drugs. He has no other medical problems. Here is his EKG. What do you want to do?
This ECG shows ST segment elevation in V2 and V3. There is some slight elevations in V1 and V4 and minor ST segment depression in II, III, and aVF.
This week’s ECG pointers isn’t so much about the ECG itself, but the management of the patient in front of you. The ECG shows ST segment elevation in V2/3. There’s also some elevation in V1 and V4 and some ST segment depression in the inferior leads. This is concerning for an anterior MI (LAD distribution), but the patient is 21 years old and just used cocaine! Does this change your management?
Let’s review what cocaine does to the body:
Cocaine causes a huge catecholaminergic surge. All those catecholamines cause vessels to clamp down (vasoconstriction). They also make the heart pump harder (inotropy) and faster (chronotropy). So, you have coronary vessels getting smaller and cardiac muscle working harder. This sounds bad. To make it even worse, the chronotropic effects of cocaine are increased when alcohol is used on top of the cocaine.
Statistically, who does cocaine? Young men who smoke.
Smoking leads to early atherosclerosis. That’s also bad. Cocaine also increases platelet count, aggregation and activation.
So, basically, the body is set up for a perfect storm. You have a heart that likely has some early atherosclerosis that now has its blood supply cut down and its oxygen requirements increased. So, is what we’re seeing on the ECG truly reflective of an acute MI?
That’s a very tough question. To answer it, we need to review some of the first studies looking at cocaine abuse and the associated ECG changes.
Back to our patient—His ECG showed ST elevation with reciprocal depressions and CODE STEMI was called. Cardiology came to the bedside, evaluated him, and decided to take him to the cath lab. The patient was found to have atherosclerosis, but no interventions were required in the cath lab. He made an uneventful recovery in the ICU and was discharged two days later.