ICU Delirium Management During SARS-CoV-2 Pandemic
pubmed.ncbi.nlm.nih.gov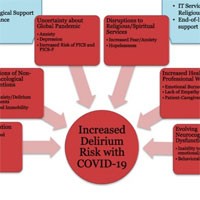
The novel coronavirus, SARS-CoV-2-causing Coronavirus Disease 19 (COVID-19), emerged as a public health threat in December 2019 and was declared a pandemic by the World Health Organization in March 2020. Delirium, a dangerous untoward prognostic development, serves as a barometer of systemic injury in critical illness.
The early reports of 25% encephalopathy from China are likely a gross underestimation, which we know occurs whenever delirium is not monitored with a valid tool.
Indeed, patients with COVID-19 are at accelerated risk for delirium due to at least seven factors including (1) direct central nervous system (CNS) invasion, (2) induction of CNS inflammatory mediators, (3) secondary effect of other organ system failure, (4) effect of sedative strategies, (5) prolonged mechanical ventilation time, (6) immobilization, and (7) other needed but unfortunate environmental factors including social isolation and quarantine without family.
Given early insights into the pathobiology of the virus, as well as the emerging interventions utilized to treat the critically ill patients, delirium prevention and management will prove exceedingly challenging, especially in the intensive care unit (ICU).
The main focus during the COVID-19 pandemic lies within organizational issues, i.e., lack of ventilators, shortage of personal protection equipment, resource allocation, prioritization of limited mechanical ventilation options, and end-of-life care.