Nasotracheal vs. Orotracheal Intubation for Sedation in Critically Ill Patients
nature.com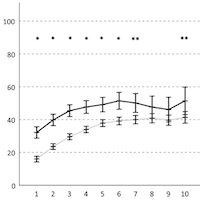
Nasotracheal intubation (NTI) may be used for long term ventilation in critically ill patients. Although tracheostomy is often favored, NTI may exhibit potential benefits. Compared to orotracheal intubation (OTI), patients receiving NTI may require less sedation and thus be more alert and with less episodes of depression of respiratory drive.
We aimed to study the association of NTI versus OTI with sedation, assisted breathing, mobilization, and outcome in an exploratory analysis. Retrospective data on patients intubated in the intensive care unit (ICU) and ventilated for > 48 h were retrieved from electronic records for up to ten days after intubation.
Outcome measures were a Richmond Agitation and Sedation Scale (RASS) of 0 or − 1, sedatives, vasopressors, assisted breathing, mobilization on the ICU mobility scale (ICU-MS), and outcome.
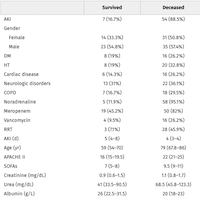
From January 2018 to December 2020, 988 patients received OTI and 221 NTI. On day 1–3, a RASS of 0 or − 1 was attained in OTI for 4.0 ± 6.1 h/d versus 9.4 ± 8.4 h/d in NTI, p < 0.001. Propofol, sufentanil, and norepinephrine were required less frequently in NTI and doses were lower.